By nature, women face a triple threat of risk factors when it comes to arthritis: biology, genetic predisposition, and hormones. Unfortunately, a lot of women have added a fourth risk factor to the mix — obesity.
Overall, women have osteoarthritis, the most common form of arthritis, at much higher rates than men. Experts estimate that almost 27 million people in the United States have osteoarthritis, and that about 60 percent of them are women. Before age 55, more men tend to have osteoarthritis, but after age 55 the number of women with the condition far surpasses the number of men.
Joints affected by osteoarthritis also tend to vary by gender, says Alexander Shikhman, MD, PhD, founder of the Institute for Specialized Medicine in Del Mar, Calif., and medical director of Restorative Remedies. Men are more prone to experience arthritis in their hips, while women tend to have it in the knees or hands, he says.
There are several reasons why these differences occur. They include:
Biology: Women’s bodies are designed to give birth, and that means the tendons in their lower body are more elastic than men’s. “As a result, the joints probably move around a little more,” says Yusuf Yazici, MD, a rheumatologist at New York University Hospital for Joint Diseases in New York. When the joints have less stability, they’re more prone to injury.
Also, because women’s hips are wider than their knees, their knee joints are not aligned as straight as men’s, Dr. Yazici says. The alignment of a woman’s body leads to a higher rate of knee injuries, and injuries can lead to osteoarthritis later in life. Experts have found that women who play soccer, for instance, have at least three to four times the number of knee injuries as men who play soccer, Yazici says.
Genetics: Osteoarthritis seems to run in families, and there appears in particular to be a genetic link among women. Women whose mothers developed osteoarthritis will probably find that they will develop it in the same joints at around the same age as she did, Yazici says. Researchers have found that hand and knee osteoarthritis have specific genetic links.
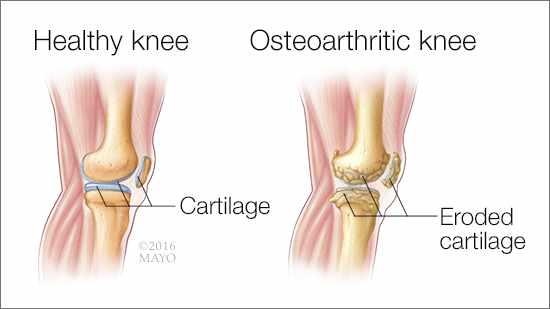
Hormones: Researchers believe that female hormones have an effect on the cartilage that sits between the bones of the joints and cushions the bones to prevent pain and allow the joints to move about smoothly. In laboratory studies of cells that form cartilage, experts have found that the female hormone estrogen protects cartilage from inflammation, Dr. Shikhman says. Inflammation can lead to osteoarthritis. But after menopause, when women’s estrogen levels go down, they lose that protection and may have a higher risk of developing osteoarthritis even if they are on hormone–replacement therapy (HRT).
A recent study of 1.3 million women in their 50s found that hormonal and reproductive factors, such as going through puberty at an early age, having more children, and taking hormone-replacement therapy, were all related to whether they had had knee or hip joint replacement surgery, but the researchers don’t know what these connections mean.
The study also found that women who started menstruating at age 11 or earlier had a 9 to 15 percent higher risk of needing hip and/or knee replacement surgery as an adult. Additionally, women who used hormone-replacement therapy after menopause were at significantly higher risk for hip and knee replacement surgery.
Giving birth was another risk factor for osteoarthritis found in this study. Researchers calculated that with each birth, the woman’s risk of needing knee replacement rose by 8 percent, and for hip replacement by 2 percent.
Although taking birth control pills seemed to have no effect on osteoarthritis risk, using HRT increased the risk that a woman would undergo knee replacement by 58 percent, and hip replacement by 38 percent. Researchers did note, however, that women who take HRT might be in more frequent contact with their doctors and may have better health care, which could explain why they were more likely to have joint replacement surgery.
Obesity: Statistics show that more women than men are obese or severely obese, and obesity plays a major role in osteoarthritis, Yazici says. Extra weight puts more pressure on joints and can cause the cartilage between joints to wear away faster. With every extra pound you gain, you add three pounds of pressure to your knees and six pounds of pressure to your hips, according to the Arthritis Foundation. Also, women who have gone through menopause tend to have more belly fat, which puts more pressure on the lower joints, Shikhman says.
Treatment
- Lose Weight. If you are overweight or obese, you’re putting extra stress on weight-bearing joints. Losing weight lessens the risk of further joint injury. It also increases your mobility.
- Work on Your Diet. If losing weight is a goal, talk to a dietitian to get on track with healthy eating habits. Also, antioxidant and calcium supplements can boost your bone strength: Vitamin D (400 IU daily) and calcium (1,000-1,200 mg daily). Antioxidant vitamins C and E may also provide bone protection.
- Stay Active. Exercise is hands-down the best treatment for osteoarthritis. Exercise helps you lose weight, increases flexibility, eases pain, boosts your mood, strengthens your heart, and improves blood flow. Mall walking, swimming, and water aerobics are popular because they are easy on joints. If exercise is painful at first, stay with it… it will get easier, reducing overall pain in the long run. But be sure to talk to your doctor before starting a new fitness or diet plan.
- Get Strong. Muscles become weak when you have osteoarthritis, and that leads to more pain. By doing exercises to strengthen muscles, you ease the pain and develop greater stability in your joints — so there’s less risk of falls. Also, special exercises can increase the range of motion in your joints. Talk to your physician or physical therapist to be sure you’re doing these exercises correctly.
- Have Fun. Don’t let your life be all about osteoarthritis. Get out, have a good time! When you’re distracted from the pain, you’ll feel happier. Sports, hobbies, volunteer projects, and other activities can take your mind off the pain. If you’re having trouble participating in favorite activities, talk to an occupational therapist about your options.
- Make Adjustments. Sensible changes can lessen the strain on joints and muscles and prevent painful spasms. If you have osteoarthritis in your back, make sure it gets good support when you sit. That means sitting in a chair to read, not reading in bed. If you have arthritis in your hip, it helps to adjust the toilet seat or furniture to a comfortable level.
- Use Heat and Cold. Heating pads, hot packs, a warm bath or shower, warm wax (paraffin) applications — these increase blood flow, easing pain and stiffness. Cold packs can reduce inflammation in a sore area. Many people keep bags of ice or frozen vegetables (like peas) on hand. Wrapped in a towel, these cold packs easily mold to fit a sore joint, like a knee.
- Take a Break. While exercise is great for helping osteoarthritis, overexertion can cause even more pain. It’s important to slow down or stop when you need to. Tune in to your body, and learn when you’re doing too much.
- Get a Soothing Massage. For treatment of pain, Americans rate massage as highly as medications. One in five adults got a therapeutic massage last year — and three-quarters of them would recommend it to others, one survey showed. Massage helps relieve pain by increasing blood flow and warmth in painful areas.
- Alternative Therapy. When conventional pain treatments don’t work, many people turn to complementary or alternative therapies. Research shows that acupuncture can help relieve joint pain by stimulating natural, pain-relieving chemicals produced by the nervous system. Glucosamine and chondroitin are well-known and researched supplements for arthritis. Both are natural substances found in joint fluid. Each is thought to stimulate the increase of cartilage production and reduce inflammation. Studies have had mixed results; one large study found that the supplement had no effect on mild osteoarthritis, but did help with moderate-to-severe arthritis. Another study found that glucosamine slowed progression of osteoarthritis in the knee.
- Use Assistive Devices. If you feel unstable on your feet — like you might fall — it’s time for a cane, walker, or knee brace. “Assistive devices help take weight off the joint and decrease pain, in addition to making you feel more stable on your feet,” says Kaur.
Source: WebMD and EverydayHealth